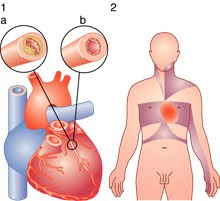
Angina pectoris is the medical term for chest pain or discomfort due to coronary heart disease. Angina is a symptom of a condition called myocardial ischemia. It occurs when the heart muscle (myocardium) doesn't get as much blood (hence as much oxygen) as it needs. This usually happens because one or more of the heart's arteries (coronary blood vessels that supply blood to the heart muscle) is narrowed or blocked. Insufficient blood supply is called ischemia.
The term derives from the Latin angina ("infection of the throat") from the Greek ἀγχόνη ankhone ("strangling"), and the Latin pectus ("chest"), and can therefore be translated as "a strangling feeling in the chest".
Typical angina is uncomfortable pressure, fullness, squeezing or pain in the center of the chest. The discomfort also may be felt in the neck, jaw, shoulder, back or arm. Many types of chest discomfort aren't related to angina. Acid reflux (heartburn) and lung infection or inflammations is examples.
Development of Angina Pectoris:
Angina pectoris is typically experienced in the symptoms of uncomfortable pressure, which feels like squeezing or pain in the center of the chest. You may also feel it in the neck, jaw, shoulder, back, arm, or stomach, including nausea.
It has been described as a tight or heavy feeling in the chest, or sometimes as pressure, squeezing, or burning. It can feel very difficult to breath, as though you are short of breath and unable to fill your lungs completely. These symptoms can be accompanied by numbness or tingling in the shoulders, arms, or wrists. However, just because you have these symptoms does not mean you have angina. You could have pericarditis, the inflammation of the sac around the heart. It might be something very serious, such as an aortic dissection, in which the inner layers of the aorta separate, causing you pain.
It might be a coronary spasm, in which the blood vessels to the heart spasm and constrict the blood flow momentarily. You may even be having a heart attack, so these painful symptoms should be evaluated by your doctor immediately. Even some non-heart related conditions can cause angina, such as heartburn, panic attacks, pleurisy (an inflammation of the chest membrane), esophageal spasms (in which the esophagus spasms causing food to back up), or simple sort muscles from improper stretching, or from conditions such as fibromyalgia. You may also have a lung infection or inflammation.
Angina, the feeling of pain or pressure, occurs when the heart needs more blood to bring it oxygen, so strenuous activity might trigger it. Running or walking quickly, carrying groceries, a rush of strong emotions, lifting something heavy, eating too much, having sex, or even extremes in temperatures, might trigger an attack. In some people, angina is caused by a condition known as coronary artery spasm, and in those cases you might feel pain or pressure even when you are resting.
Classification of Angina Pectoris:
There are two major different types of angina pectoris. There’s stable angina, and in these cases, the angina is usually predictable and you can expect to have symptoms in consistent situations (every time you run, every time you get angry, etc). Unstable angina means that the pain takes you by surprise, and can occur when you are at rest. With unstable angina, the chest pain can be more severe and prolonged than with stable angina. Both of these conditions can be caused by reduced blood flow to the heart muscles because of blockage by fatty build-ups. This blockage is called arterioschlerosis.
Stable angina:
Also known as effort angina, this refers to the more common understanding of angina related to myocardial ischemia. Typical presentations of stable angina is that of chest discomfort and associated symptoms precipitated by some activity (running, walking, etc.) with minimal or non-existent symptoms at rest. Symptoms typically abate several minutes following cessation of precipitating activities and resume when activity resumes. In this way, stable angina may be thought of as being similar to claudication symptoms.
People with stable angina (or chronic stable angina) have episodes of chest discomfort that are usually predictable. They occur on exertion (such as running to catch a bus) or under mental or emotional stress. Normally the chest discomfort is relieved with rest, nitroglycerin or both.
People with episodes of chest discomfort should see their physician for an evaluation. The doctor will evaluate the person's medical history and risk factors, conduct a physical exam, order a chest X-ray and take an electrocardiogram (ECG). Some people will also need an exercise ECG (stress test), an echocardiogram or other tests to complete the diagnosis.
Unstable angina:
Unstable angina (UA) (also "crescendo angina;" this is a form of acute coronary syndrome) is defined as angina pectoris that changes or worsens.
It has at least one of these three features:
- it occurs at rest (or with minimal exertion), usually lasting >10 min;
- it is severe and of new onset (i.e., within the prior 4–6 weeks); and/or
- it occurs with a crescendo pattern (i.e., distinctly more severe, prolonged, or frequent than previously).
UA may occur unpredictably at rest which may be a serious indicator of an impending heart attack. What differentiates stable angina from unstable angina (other than symptoms) is the pathophysiology of the atherosclerosis. The pathophysiology of unstable angina is the reduction coronary flow due to transient platelet aggregation on apparently normal endothelium, coronary artery spasms or coronary thrombosis. The process starts with atherosclerosis, and when inflamed leads to an active plaque, which undergoes thrombosis and results in acute ischemia, which finally results in cell necrosis after calcium entry. Studies show that 64% of all unstable anginas occur between 10 PM and 8 AM when patients are at rest.
In people with unstable angina, the chest pain is unexpected and usually occurs while at rest. The discomfort may be more severe and prolonged than typical angina or be the first time a person has angina. The most common cause is reduced blood flow to the heart muscle because the coronary arteries are narrowed by fatty buildups (atherosclerosis). An artery may be abnormally constricted or partially blocked by a blood clot. Inflammation, infection and secondary causes also can lead to unstable angina. In a form of unstable angina called variant or Prinzmetal's angina, the cause is coronary artery spasm.
Major risk factors:
- Age (≥ 55 yo for men, ≥ 65 for women)
- Cigarette smoking
- Diabetes mellitus (DM)
- Dyslipidemia
- Family History of premature CVD
- Hypertension (HTN)
- Kidney disease
- Obesity (BMI ≥ 30 kg/m2)
- Physical inactivity
- Smoking
Other Medical Problems by Angina Pectoris:
- profound anemia
- uncontrolled HTN
- hyperthyroidism
- hypoxemia
- tachyarrhythmia
- bradyarrhythmia
- valvular heart disease
- hypertrophic cardiomyopathy
Prevention of Angina Pectoris:
Unlike some diseases, however, angina can be stopped before it even gets started. It is quite preventable, but even if you haven’t prevented it, you can reduce it through some basic lifestyle changes. First, stop smoking. Smokers have more than double the risk of heart attacks and strokes than non-smokers, and heavy smokers have more than twice the risk of light smokers. Adopt healthier eating habits; avoid trans fats, saturated fats, cholesterol, and salt. A healthier diet will also help you control your blood pressure and overall cholesterol levels. Another overlooked lifestyle change concerns stress; can you relax, even when life is challenging? Learn to breathe deeply to keep oxygen flowing, which is necessary both to your heart and your feeling of well-being.
While it’s true that making good lifestyle choices can go far in preventing the heart disease that angina signals, it’s also true that some people are just prone to it because of their family history. Make sure to tell your doctor if anyone in your family has had heart disease or a heart attack or stroke. This information will help your doctor decide when and how to treat your angina.
Signs and Symptoms:
Most patients with angina complain of chest discomfort rather than actual pain: the discomfort is usually described as a pressure, heaviness, tightness, squeezing, burning, or choking sensation. Apart from chest discomfort, anginal pains may also be experienced in the epigastrium (upper central abdomen), back, neck area, jaw, or shoulders. This is explained by the concept of referred pain, and is due to the spinal level that receives visceral sensation from the heart simultaneously receiving cutaneous sensation from parts of the skin specified by that spinal nerve's dermatome, without an ability to discriminate the two. Typical locations for referred pain are arms (often inner left arm), shoulders, and neck into the jaw. Angina is typically precipitated by exertion or emotional stress. It is exacerbated by having a full stomach and by cold temperatures. Pain may be accompanied by breathlessness, sweating and nausea in some cases. In this case, the pulse rate and the blood pressure increases. The pain usually lasts for about 3 to 5 minutes but the symptoms actually starts 15 to 20 minutes before the cardiac arrest and the pain is relieved by rest or specific anti-angina medication. Chest pain lasting only a few seconds is normally not angina.
Myocardial ischemia comes about when the myocardia (the heart muscles) receive insufficient blood and oxygen to function normally either because of increased oxygen demand by the myocardia or by decreased supply to the myocardia. This inadequate perfusion of blood and the resulting reduced delivery of oxygen and nutrients is directly correlated to blocked or narrowed blood vessels.
Treatment of Angina Pectoris:
The most specific medicine to treat angina is nitroglycerin. It is a potent vasodilator that makes more oxygen available to the heart muscle. Beta-blockers and calcium channel blockers act to decrease the heart's workload, and thus its requirement for oxygen. Treatments are baloon angioplasty, in which the balloon is inserted at the end of a catheter and inflated to widen the arterial lumen. Stents to maintain the arterial widening are often used at the same time. Coronary bypass surgery involves bypassing constricted arteries with venous grafts. This is much more invasive than angioplasty.
The main goals of treatment in angina pectoris are relief of symptoms, slowing progression of the disease, and reduction of future events, especially heart attacks and, of course, death. Beta blockers (e.g., carvedilol, propranolol, atenolol) have a large body of evidence in morbidity and mortality benefits (fewer symptoms, less disability and longer life) and short-acting nitroglycerin medications have been used since 1879 for symptomatic relief of angina. Calcium channel blockers (such as nifedipine (Adalat) and amlodipine), isosorbide mononitrate and nicorandil are vasodilators commonly used in chronic stable angina [citation needed]. A new therapeutic class, called If inhibitor, has recently been made available: ivabradine provides pure heart rate reduction leading to major anti-ischemic and antianginal efficacy. ACE inhibitors are also vasodilators with both symptomatic and prognostic benefit and, lastly, statins are the most frequently used lipid/cholesterol modifiers which probably also stabilize existing atheromatous plaque [citation needed]. Low-dose aspirin decreases the risk of heart attack in patients with chronic stable angina, and was previously part of standard treatment, however it has since been discovered that the increase in haemorrhagic stroke and gastrointestinal bleeding offsets this gain so they are no longer advised unless the risk of myocardial infarction is very high.